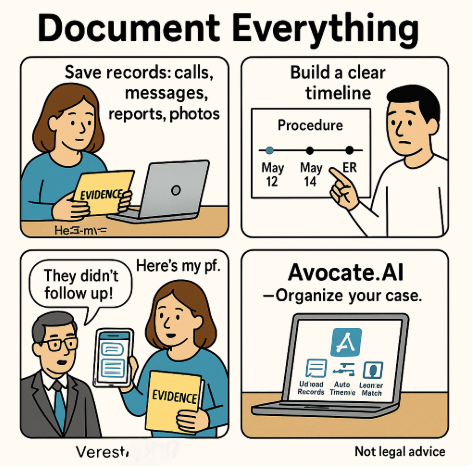
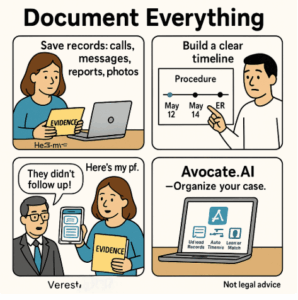
 Short version: if it isn’t written down, saved, dated, and backed up, it’s much harder to prove. Defense teams often argue you missed follow-ups, ignored instructions, or had a pre-existing problem. Careful, consistent documentation is how you push back and win credibility.
Short version: if it isn’t written down, saved, dated, and backed up, it’s much harder to prove. Defense teams often argue you missed follow-ups, ignored instructions, or had a pre-existing problem. Careful, consistent documentation is how you push back and win credibility.
Disclaimer: This post is general information, not legal advice. If you believe you were harmed by medical negligence, consult a licensed attorney in your state as soon as possible—deadlines (statutes of limitations) are strict.
Why documentation wins cases
In medical cases, the side with the clearer paper trail is usually more believable. Your records and notes:
-
Rebut “patient non-compliance” claims (e.g., “they never returned”).
-
Show causation (symptoms changed after a specific act/omission).
-
Preserve details that fade from memory.
-
Help experts reconstruct what happened and when.
Common defense arguments—and how your evidence counters them
-
“You missed follow-ups / didn’t follow instructions.”
Counter: Appointment confirmations, calendar entries, call logs, portal messages, written instructions you followed, pharmacy refill history. -
“This was a known complication, not negligence.”
Counter: Informed-consent forms (what risks were disclosed), alternative safer options discussed (or not), expert notes indicating deviation from guidelines. -
“Symptoms were pre-existing.”
Counter: Baseline records and journals showing you were symptom-free or stable before the event. -
“No causation—unrelated to what we did.”
Counter: Timeline that precisely links the procedure/medication to onset or worsening of symptoms; second-opinion notes connecting dots.
The 48-Hour “Start Now” Checklist
-
Write a timeline (dates + times): first symptoms ⇒ visits/tests ⇒ treatments ⇒ outcomes. Keep it factual and calm.
-
Secure all communications: texts, emails, patient-portal messages, voicemails. Screenshot with visible timestamps; save to PDF.
-
Request your records (see “Records 101” below). Ask for the full chart, not just a “summary.”
-
Photograph injuries daily under consistent lighting. Add the date to the filename.
-
Journal symptoms & impact (pain scale, mobility limits, missed work, life activities affected).
-
Gather financial proof: bills, EOBs, out-of-pocket receipts, travel costs, lost-wage documentation.
-
Back up everything to at least two places (e.g., encrypted cloud + USB).
Do not alter anything (no edits to photos metadata, no changing journal entries after the fact). Authenticity matters.
What to collect (specifics)
Medical records
-
Admission/discharge summaries, progress notes, nursing notes, operative report, anesthesia record, medication administration record (MAR), orders, vital signs, triage notes.
-
Imaging & raw data: Radiology reports and actual images (DICOM on CD/USB).
-
Lab results with reference ranges; pathology reports.
-
Informed consent forms for procedures.
-
Device details: Implant cards, serial numbers, packaging if available.
Communications
-
Patient-portal messages and attachments (export or screenshot).
-
Emails/texts with providers or schedulers.
-
Call logs (date/time, number). Keep a phone-call diary (who, what, when).
Medications
-
Prescription labels, pharmacy printouts, refill history, drug info sheets, pill bottles/packaging.
Personal documentation
-
Daily symptom journal (brief but consistent).
-
Photos/videos of visible injuries, rashes, swelling, mobility limits.
-
Witness info (family/friends who saw your condition before/after).
Financial impact
-
Time off work (employer letters, pay stubs), freelance cancellation emails, mileage to appointments, childcare costs.
Records 101: How to request the right stuff
Under HIPAA, you’re entitled to your medical records. To speed things up:
-
Ask for “the complete medical record for [dates]” including:
-
Progress notes, nursing notes, orders, MAR, vitals, labs, imaging reports and images, op/anesthesia reports, consults, discharge instructions, consent forms.
-
-
Also request the EMR “audit log” (access log/metadata) if you suspect record changes—this can show who edited what and when.
-
Request format: PDF for text; DICOM for imaging; machine-readable files if offered.
-
Keep a log of each request: date sent, contact person, response received.
-
Follow up in writing if deadlines lapse; keep copies.
Tip: You don’t need to explain why you want records. Be polite, precise, and persistent.
If you’re still receiving care
-
Safety first: Don’t halt necessary treatment. Seek a second opinion with a new provider (bring your timeline and key records).
-
Be factual with staff. Avoid arguments; ask that concerns be “noted in the chart.”
-
Get written instructions for home care and follow them; photograph the discharge papers.
-
Mind the law on recordings: Some states require all-party consent—ask a lawyer before recording conversations.
What not to do
-
Don’t post about your case on social media.
-
Don’t sign broad releases from insurers or hospitals without legal review.
-
Don’t “fix” typos in your journal, edit image timestamps, or recreate missing items.
-
Don’t accept quick settlement offers before you understand the full harm and future costs.
Two quick examples
-
Missed follow-up smear → late cancer diagnosis
A patient kept portal reminders, a call log of rescheduling attempts, and screenshots of a clinic cancellation. When the defense argued “no follow-up,” her records showed she tried three times and followed the written plan. -
Post-op infection downplayed
Daily photos documented wound changes and fever logs; pharmacy records confirmed antibiotics filled and taken. The timeline plus MAR showed delayed antibiotic coverage despite reported symptoms—key for establishing breach and causation.
Timing matters—don’t wait
Medical malpractice deadlines can be short and complex (statutes of limitation and repose, special rules for minors or public hospitals). Early review preserves evidence and keeps your options open.
How Avocate.AI can help
If you’re overwhelmed by the paperwork—totally normal—Avocate.AI can lighten the load:
-
Secure evidence vault to upload records, images, messages, and receipts.
-
Automatic timeline builder from documents, timestamps, and metadata.
-
Medical insight: flags likely deviations from standards of care for expert review.
-
Case readiness report you can share with counsel.
-
Lawyer match: connects you with a vetted, competent trial lawyer in your jurisdiction.
Next step: Gather the items above, then contact Avocate.AI ( contact@avocate.ai). The sooner your evidence is organized, the stronger your position—and the faster a qualified trial lawyer can evaluate and pursue your claim.